Antithrombotic agents (anticoagulants and antiplatelets)
| Type | Recommendation |
|---|---|
| When to deprescribe | |
| CBR |
We suggest deprescribing be offered to older people taking anticoagulants:
We suggest deprescribing of warfarin be offered to older people with advanced chronic kidney disease (CKD IV-V/ESKD) as the risk of complications may outweigh the potential benefits of anticoagulation. |
| CBR |
We suggest deprescribing of antiplatelets be offered to older people:
provided the person is stable and the risks of bleeding outweigh the benefits of continued dual therapy. |
| GPS |
Deprescribing decisions should be made in consultation with the person and their GP and/or specialist providers to ensure it aligns with their preferences, goals and overall treatment plans (ungraded good practice statement). |
| Ongoing treatment | |
| CBR |
We suggest continuing antithrombotics in robust older people with cardiovascular risk factors taking:
provided there are no life-limiting diseases (where potential risks often outweigh potential benefits) or significant bleeding risk, and this aligns with the individual's goals and preferences, following informed consent. |
| GPS |
Healthcare providers should reassess an individual’s cardiovascular and bleeding risk at least annually or more frequently, based on clinical indications or changes in health status, using a validated tool appropriate for the patient population (e.g. HAS-BLED for estimating major bleeding risk in people receiving anticoagulation for atrial fibrillation, and CHA2DS2-VASc for calculating stroke risk) (ungraded good practice statement). |
| How to deprescribe | |
| CBR |
We suggest ceasing anticoagulants and/or antiplatelets, without the need for tapering. |
| Monitoring | |
| CBR |
Routine monitoring We suggest close monitoring of ongoing risk factors (e.g. risk of bleeding and cardiovascular events), at least monthly for the first six months after deprescribing, followed by monitoring every six months thereafter to maintain the therapeutic relationship while working on potentially modifiable cardiovascular risk factors through lifestyle optimisation. However, this should be tailored based on individual factors such as their preferences, responses and tolerance to deprescribing. For warfarin, routine monitoring of the international normalised ratio (INR) when stopping is generally not required, especially if the INR is within the therapeutic range. However, closer monitoring (a few days after cessation) may be preferred if there are concurrent illnesses or medicine changes (including prescribed, over-the-counter medicines, complementary and alternative medicines). For people who need to restart warfarin therapy, closely monitoring the INR is essential to achieve the therapeutic range. |
| CBR |
We suggest advising people to present for medical attention in case of concerning symptoms (e.g. dyspnoea, chest pain, or painful and/or swollen calf suggestive of venous thromboembolism). |
CBR, consensus-based recommendation; GPS, good practice statement
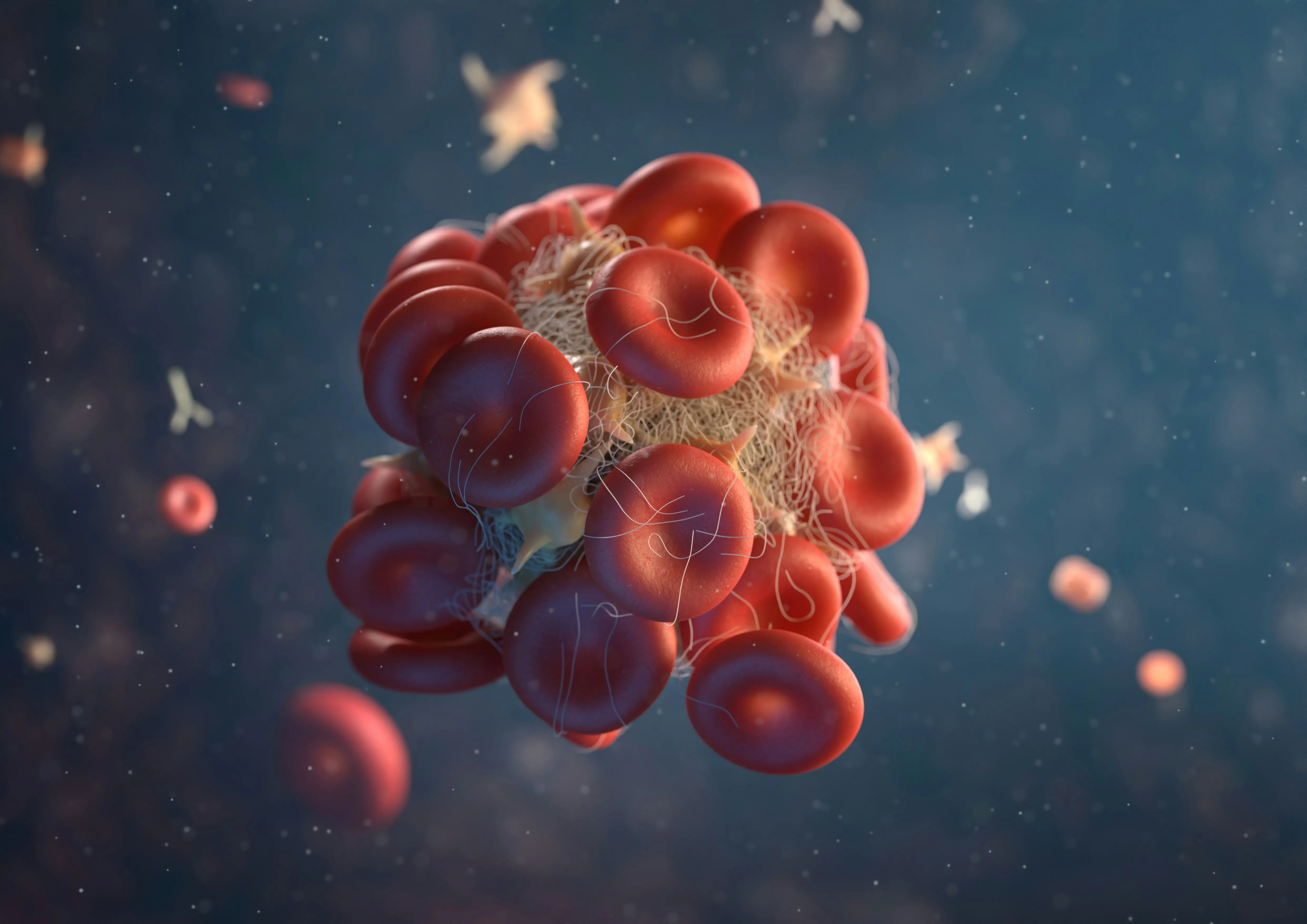
Anticoagulants
Anticoagulants are indicated for deep vein thrombosis, pulmonary embolism, ischaemic stroke, transient ischaemic attack, and during the acute hospitalisation phase of acute coronary syndromes (ACS) [211]. Independent risk factors for the long-term risk of major bleeding include age > 65 years, concomitant antiplatelet therapy, renal impairment (creatinine clearance < 50 mL/min), anaemia, and history of major bleeding [271, 272]. In clinical practice, anticoagulants for stroke prevention are often under-prescribed in older people with newly diagnosed atrial fibrillation (AF), likely due to the perceived risk of severe haemorrhage outweighing anticoagulation benefits [273, 274].
The factors influencing the prescribing of direct oral anticoagulants and warfarin in older people with AF include a history of dementia, falls, major bleeds, and fractures [275]. Optimal prescribing of anticoagulants requires the healthcare provider to assess the benefits of reduced thromboembolic events against the risk of major bleeding. In people who require long-term anticoagulation, at least an annual reassessment of risks and benefits is essential [271]. Excessive anticoagulation may lead to serious harm including anticoagulant-related nephropathy and bleeding [211]. Anticoagulant-related nephropathy is a type of acute kidney injury, but it may also result in permanent kidney damage and increased mortality [211].
Antiplatelets
Antiplatelets are indicated for the prevention of ACS or cerebral vascular disease [211]. Its use can be separated into primary (without established cardiovascular disease) or secondary prevention (with a prior cardiovascular event).
Dual antiplatelet therapy (DAPT)
Other antiplatelet agents (P2Y12 antagonists e.g. clopidogrel, ticagrelor, prasugrel) are often used as secondary prevention agents to prevent the recurrence of cardiovascular events. DAPT, consisting of aspirin and P2Y12 receptor antagonists, is often initiated post-hospitalisation for ACS or stroke. Recommended duration varies depending on the initial indication, and individual bleeding and ischaemic risks.
The 2025 Australian clinical guideline for the diagnosis and management of ACS provided a strong recommendation that DAPT (with aspirin and a P2Y12 inhibitor) should be prescribed for [276]:
- Six to 12 months in people discharged post-ACS who are at high ischaemic and/or low bleeding risk
- One to three months post-ACS in low ischaemic and/or high bleeding risk, followed by single antiplatelet therapy (SAPT)
In addition, the 2025 American College of Cardiology (ACC) and American Heart Association (AHA) joint guideline for the management of ACS provides updated recommendations on dual antiplatelet therapy (DAPT) duration and strategies to reduce the risk of bleeding [277]:
- For people not at high bleeding risk, a standard 12-month DAPT regimen consisting of aspirin and an oral P2Y12 inhibitor is recommended to reduce the risk of major adverse cardiovascular events (MACE)
- In patients with ACS who have tolerated DAPT (aspirin and ticagrelor), discontinuation of aspirin and continuation with ticagrelor monotherapy after one to three months post-PCI may be considered to lower bleeding risk. Alternatively, de-escalation of P2Y12 inhibitor potency (from aspirin + ticagrelor/prasugrel to aspirin + clopidogrel) can be considered to reduce bleeding risk
- In patients with ACS at high bleeding risk, early transition to single antiplatelet therapy (either aspirin or a P2Y12 inhibitor) after one month post-PCI may be reasonable
Evidence supports shortened DAPT durations in selected post-PCI populations to balance the risks of bleeding and MACE. A 2024 systematic review and meta-analysis of 14 RCTs found that abbreviated DAPT regimens of one or three months were associated with significantly lower bleeding risk compared to six months of DAPT, without an increase in net adverse clinical events or MACE [278]. Additionally, three months of DAPT was associated with a lower risk of bleeding compared to 12 months [278]. Additionally, when comparing aspirin monotherapy with clopidogrel monotherapy, a secondary analysis of the STOPDAPT-3 trial found no significant difference in cardiovascular or bleeding outcomes beyond 1 month and up to 12 months after PCI with drug-eluting stents [279].
Concurrent antiplatelet and anticoagulant therapy
Certain clinical situations necessitate the temporary use of combined antiplatelet therapy and oral anticoagulants (OAC), after which a clinical decision should be made to discontinue either therapy. Combining antiplatelet with OAC should only occur in people who require anticoagulation for thromboembolic prevention (e.g. AF, venous thromboembolism) but also have an indication for antiplatelet therapy (e.g. recent ACS or percutaneous coronary intervention) [280].
Triple antithrombotic therapy (an oral anticoagulant, aspirin and a P2Y12 inhibitor) is commonly indicated for people requiring long-term anticoagulation therapy (e.g. for AF, venous thromboembolism, and prosthetic heart valves) plus an indication for dual antiplatelet therapy following coronary stent insertion for ACS. The balance between ischaemic and bleeding risks must be carefully considered.
Refer to the narrative evidence summary, the GRADE Summary of Findings table in the guidelines, and the Technical Report for a complete presentation of the deprescribing evidence based on the GRADE framework (including other factors considered in developing the recommendations).
1. Anticoagulants
Although AF primarily affects older people, they are often under-represented in RCTs, particularly those who are frail. Australian clinical guidelines recommend anticoagulation for all people aged 75 years and older with non-valvular AF [281]. In people with acute ischemic stroke and AF, OAC is often switched to antiplatelet therapy until the risk of haemorrhagic transformation is low, normally up to two weeks, depending on the size of the infarcted area, after which the OAC is re-started [282]. The risk of major bleeding in people taking OAC for stroke prophylaxis is 2-3% per year, with approximately half of these events being gastrointestinal bleeding [283]. Similar rates were observed when OAC was used for venous thromboembolism prophylaxis [284]. However, anticoagulant-related major bleeding is more likely to be fatal than recurrent venous thromboembolism [272]. In people with AF, anticoagulation is only recommended when the net clinical benefit of reducing ischaemic stroke risk outweighs the potential harm from major bleeding. The bleeding risk in people prescribed long-term anticoagulation for atrial fibrillation can be estimated using the HAS-BLED score. In older people with advanced chronic kidney disease (CKD IV-V/ESKD), the risk of bleeding complications with warfarin use often outweighs the potential benefits of anticoagulation [285].
CHA2DS2-VASc is a point-based tool that can be used to calculate stroke risk in people with atrial fibrillation [286]. The tool was validated to predict the patients at high risk for mortality within three to five years in people with atrial fibrillation [286]. The scores for stratifying risk levels were score 0 (low risk), score 1 (medium risk), and score ≥ 2 (high risk) [286]. For people with a CHA2DS2–VASc score of ≥ 2 (high risk), anticoagulant therapy is recommended, whereas in those with a CHA2DS2-VA score of 1 (medium risk), anticoagulant therapy should be considered following a person-centred approach and careful assessment of other thromboembolic risk factors if present [280].
However, the tools are not sufficient on their own to justify withholding anticoagulants in AF [281]. A study involving approximately 25,000 people with AF found that for those with a HAS-BLED score of 3 or more, continuing OAC was associated with better clinical outcomes, including stroke prevention, reduced major bleeding, and lower all-cause mortality [287]. Higher HAS-BLED scores may be used as a prompt to identify and address modifiable bleeding risk factors, such as uncontrolled hypertension, excessive alcohol intake, concomitant antiplatelet use, and the need for fall prevention. Restarting anticoagulation after a bleeding episode must balance stroke prevention with the risk of recurrent bleeding. A systematic review reported that many people with AF were willing to accept a moderate increase in the risk of bleeding to reduce stroke risk [288]. However, recommendations for clinical practice are rarely straightforward, especially in the care of people who are frail. An individualised approach should be implemented, involving informed decision-making with the person, their carer and/or family.
The anticoagulant effect of warfarin diminishes upon cessation, with normal coagulation typically restored in a few days. Warfarin has a mean half-life of 40 hours and the duration of effect is typically two to five days [289]. When stopping warfarin, routine monitoring of the international normalised ratio (INR) is generally not required, particularly if the INR is within the therapeutic range at the time of discontinuation. However, closer monitoring a few days after cessation may be appropriate in the presence of concurrent illness or changes in medications, including prescribed, over-the-counter, complementary, or alternative therapies. For individuals who require reinitiation of warfarin, close INR monitoring is essential to ensure a return to and maintenance of the therapeutic range.
For acute venous thromboembolism, anticoagulant therapy is typically prescribed for a short term, usually between six weeks and three months, depending on the clinical context [290]. Extended therapy beyond three months may be considered after a first unprovoked proximal deep vein thrombosis or pulmonary embolism, or in individuals with persisting provoking factors such as immobility, active cancer, or inflammatory bowel disease, to reduce the risk of recurrence [290]. The optimal duration of extended anticoagulation remains uncertain. Decisions to continue therapy should balance the risk of bleeding against the risk of recurrence, while also considering individual preferences.
2. Antiplatelets
Older people who are otherwise well, functionally independent, and have a life expectancy of five years or more are likely to derive the most benefits from antiplatelet therapy as secondary prevention [291]. However, the net benefit in primary prevention declines with advanced age due to underlying comorbidities. In older people without a history of cardiovascular, cerebrovascular, or peripheral arterial disease, the risk of major gastrointestinal or intracranial bleeding from aspirin often offsets the risk reduction in preventing cardiovascular events [211].
The ASPirin in Reducing Events in the Elderly (ASPREE) trial included 19,114 community-dwelling older people aged 70 years or above in Australia and the United States without a history of dementia or cardiovascular disease [292]. The study reported no benefit of prophylactic aspirin in lowering cardiovascular risk but resulted in a significantly higher risk of major bleeding events [293].
Furthermore, post-hoc subgroup analysis of the ASPREE trial demonstrated aspirin did not improve outcomes in older people with CKD while increasing bleeding risks [294]. CKD was defined as either baseline eGFR <60mL /min/1.73m2 or urine albumin to creatinine ratio> 3 mg/mmol.
The routine use of aspirin for primary prevention of cardiovascular disease in patients with chronic kidney disease is generally not recommended [295]. This is due to an increased bleeding risk in people with chronic kidney disease and clear benefit in the reduction of cardiovascular events lacking for primary prevention.
Coronary artery calcium (CAC) scoring, used for predicting future cardiovascular risk, may be useful in identifying a subgroup of people who are more likely to benefit from antiplatelet therapy for primary prevention. People with a CAC score of more than 100 were estimated to have a favourable risk/benefit profile for aspirin use in the primary prevention of coronary heart disease, with the greatest benefit observed in those with a score exceeding 400. However, these effects have not been well studied in people over the age of 70 [296, 297].
The use of DAPT beyond six to 12 months (or beyond one to three months in certain people post-PCI) is rarely indicated [276, 277], as it increases bleeding risk without additional benefit in reducing cardiovascular or all-cause mortality for most people [298]. However, individual assessment of bleeding and ischemic risk is essential to guide DAPT duration. For stroke, DAPT is recommended to be used for only 21 days following an acute ischaemic stroke or transient ischaemic attack. A meta-analysis of four trials has found the net benefit of DAPT occurred within the first 21 days and DAPT beyond three months significantly increased bleeding and mortality risk with no reduction in major vascular events [299]. DAPT therapy to reduce ischaemic risks needs to be weighed against the higher bleeding risk and all-cause mortality [298]. The PRECISE-DAPT score, validated in 21 studies, was developed to assess bleeding risk in people treated with DAPT following coronary stent insertion for coronary artery disease. Older people with either prior bleeding, anaemia Hb < 100g/L or CKD stage IV or V are recommended to have a shortened DAPT duration [300].
3. Concurrent antiplatelet and anticoagulant therapy
In people with an indication for oral anticoagulation (e.g. AF) undergoing percutaneous coronary intervention, triple therapy should be continued for up to seven days or extended up to one month in people at high ischaemic risk [277]. After this, the person should transition (i.e. step down) to OAC plus SAPT, preferably with a P2Y12 inhibitor (clopidogrel) due to its lower bleeding risk, for up to six months (in people not at high ischaemic risl) or 12 months (in people at high ischaemic risk) post-event (including duration of triple therapy), then stepping down to OAC alone ongoing for the oral anticoagulation indication [276, 277, 301]. During the first 12 months of therapy, any new ischemic or bleeding event should prompt a re-evaluation of antithrombotic therapy [281].
To date, only two RCTs have evaluated the efficacy of OAC monotherapy versus OAC plus SAPT for maintenance thrombotic prevention in people with AF, both conducted in Asian populations. The OAC-ALONE trial was terminated prematurely due to slow enrolment [302]. The AFIRE trial which followed 2,236 people over 23 months, compared rivaroxaban monotherapy with rivaroxaban plus SAPT (either aspirin or a P2Y12 inhibitor) was also stopped early due to increased mortality in the combination therapy group [303].
Several ongoing RCTs are expected to provide further insights into this area, including SoSTART, APACHE-AF, and ASPIRE trials. Although the evidence remains inconclusive, some guidelines, such as those from the European Society of Cardiology [304] and the National Heart Foundation of Australia [281], recommend OAC monotherapy for stroke prevention after six to 12 months of stenting in people with AF.
We identified one study related to anticoagulant deprescribing from the systematic review and meta-analysis [305]. Additionally, we identified five studies (two cohort studies and three before-and-after studies) related to antiplatelet deprescribing [293, 306-309].
Overall, the current evidence supporting the deprescribing of antithrombotic agents is of very low certainty. Available studies suggest that discontinuing low-dose aspirin used for primary prevention in patients without cardiovascular comorbidities may reduce the risk of mortality and bleeding. In contrast, for individuals with cardiovascular comorbidities, stopping low-dose aspirin prescribed for secondary prevention may increase the risk of mortality or acute cardiovascular events, particularly within the first six months of discontinuation. However, there is a lack of quality evidence to inform evidence-based recommendations. If deprescribing is considered appropriate, close monitoring of ongoing risk factors, such as bleeding risk and cardiovascular risk, is essential. Regular follow-up, ideally at least monthly during the first six months may be necessary while concurrently addressing modifiable cardiovascular risk factors through lifestyle optimisation.
Key study characteristics and results
A narrative summary of each study is provided below, highlighting key characteristics and main findings.
Anticoagulants
Patel 2013 reported a post-hoc analysis of a double-blind RCT comparing rivaroxaban and warfarin in people with nonvalvular AF who subsequently transitioned to open-label therapy (most commonly warfarin) at the conclusion of the study. This study compared the incidence of stroke or non-central nervous system embolism during the transition in participants previously treated with rivaroxaban versus warfarin of which both groups had a temporary interruption of therapy. The rivaroxaban group had poor anticoagulant coverage through the transition, whereas the warfarin group had no uncovered period, as evidenced by the time to a therapeutic INR. There were significantly more acute cardiovascular events (defined as ischemic stroke, non-central nervous system embolism, myocardial infarction, or vascular death) in the group that transitioned from rivaroxaban to open-label therapy at the end of the blinded RCT (compared to the warfarin group that continued open-label therapy; OR 3.73, 95% CI 1.51 to 9.21). There were also significantly more major bleeding events in the group that discontinued rivaroxaban and transitioned to open-label therapy, compared to the warfarin group that continued open-label therapy (OR 3.64, 95% CI 1.57 to 8.42).
Antiplatelets
Derogar 2013 [306] reported the discontinuation of low-dose aspirin therapy in 118 patients who were hospitalised for bleeding peptic ulcers. Among older patients with cardiovascular comorbidities (n = 76), discontinuation of low-dose aspirin therapy was associated with a substantial increase in the risk of death or acute cardiovascular events within the first six months of follow-up (OR 10.67, 95% CI 2.07, 55.07). Cardiovascular comorbidities included chronic ischemic heart disease or angina, chronic heart failure, previous myocardial infarction, AF, previous stroke or transient cerebral ischemia. However, there was no significant difference in mortality after the initial six-month follow-up (median follow-up duration of 24 months) (OR 0.97, 95% CI 0.32, 2.95). This retrospective cohort study did not report such an association in death or acute cardiovascular events in patients without any cardiovascular comorbidities. Among patients without cardiovascular comorbidities (n = 42), there was no death or acute cardiovascular events within the first six months of follow-up. Again, after the initial six-month follow-up, there was no significant difference in mortality between the two groups (OR 1.87, 95% CI 0.39, 9.12).
Sambu 2011 [307] included 33 patients who were taking low-dose aspirin clopidogrel 75 mg and statin treatment who had undergone PCI with a drug-eluting stent and were due to discontinue clopidogrel at one year. Following clopidogrel discontinuation, an increase in markers of platelet reactivity was observed. Although more evidence is required, discontinuation of clopidogrel may lead to a clustering of adverse events attributed to the increasing platelet activity after discontinuation.
Ramos 2024 [308] reported a pharmacist-led deprescribing before-and-after study conducted in a hospital outpatient setting. Patients aged 70 years or older who were taking aspirin for primary prevention without a documented history of atherosclerotic cardiovascular disease were contacted by pharmacists. These patients engaged in discussions with pharmacists regarding the risks and benefits of aspirin for primary prevention and were offered the option to discontinue its use. Of the 131 participants who met the eligibility criteria and were contacted, 78 (60%) discontinued aspirin following their consultation with a pharmacist.
Varghese 2024 [309] described a study involving veterans in a primary care setting who were aged 70 years or older and were taking aspirin for primary prevention of atherosclerotic cardiovascular disease. Participants were excluded if they were prescribed clopidogrel or had other indications for aspirin use. The control group received education from primary care providers on the risks and benefits of aspirin for primary prevention in older veterans. In the intervention group, in addition to provider education, a pharmacist discussed the risks and benefits of aspirin use with each eligible patient. Among the 57 patients who received care from the control group’s primary care providers, 10 (18%) discontinued aspirin by the end of the four-month study. Compared with the control group, a significantly greater proportion of patients in the intervention group who were contacted by a pharmacist discontinued aspirin (35/65, 54%, p = 0.0001).
Zhou 2024 [293] conducted a post-hoc analysis of the ASPREE trial using a target trial emulation framework. As previously noted, the ASPREE trial included community-dwelling older people aged 70 years or above in Australia and the United States who had no history of dementia or cardiovascular disease. The current study analysed data from 6,103 participants during the immediate post-trial period (2017–2021), identifying 5,427 participants who had discontinued aspirin and 676 who had continued its use. At 48 months, no significant difference was observed between the discontinuation and continuation groups for cardiovascular disease (OR 0.75, 95% CI 0.54, 1.03) or major adverse cardiovascular events (OR 0.88, 95% CI 0.60, 1.30). Participants in the discontinuation group had a significantly lower risk of major bleeding events (OR 0.64, 95% CI 0.42, 0.99) and all-cause mortality (OR 0.69, 95% CI 0.53, 0.90). However, after propensity score adjustment, there was no significant difference in all-cause mortality between the two groups at 48 months (HR 0.79, 95% CI 0.61, 1.03).
The method of deprescribing was not described in all studies, but it appears to have involved abrupt discontinuation.